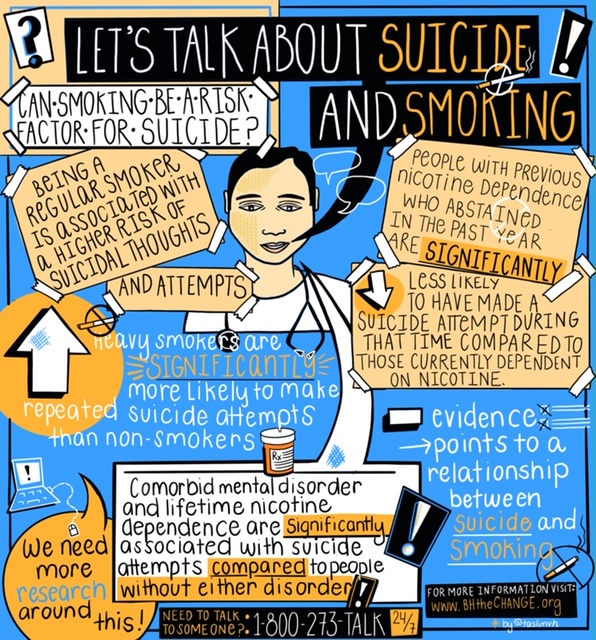
Cancer, heart disease, asthma – these are just some of the risks from smoking that have become common knowledge and they’re all risks that show smoking can be deadly, but can smoking be a risk factor for suicide too? Various studies have shown a relationship, although still emerging in our understanding, between tobacco use and suicide risk including:
- People with low nicotine dependence have lower odds of suicidal thoughts and attempts compared to people with high nicotine dependence 1
- Being a regular smoker is associated with a higher risk of suicidal thoughts and attempts 1,4
- Being highly nicotine dependent increases the odds of suicidal thoughts and attempts 1, 4
In addition to a higher risk of suicidal thoughts, studies have found some relationship between repeat attempts and smoking, such as:
- Heavy smokers are significantly more likely to make repeated suicide attempts than non-smokers 4
- People with previous nicotine dependence who had abstained in the past year are significantly less likely to have made a suicide attempt in the past year compared to those currently dependent on nicotine 2
- Co-morbid mental disorder and lifetime nicotine dependence are significantly associated with suicide attempts compared to people without either disorder 2
- $1 increase in tobacco tax was associated with 12.4% reduction in suicide rates among adults 18-65-years old 3
With emerging evidence pointing to a relationship between smoking and suicide risk -let’s start talking about it–we know talking about suicide can help! Below you will find a digest of available resources and information relating to suicide prevention to better help your patients and potentially save a life.
General Resources/ Information
- Mental Health First Aid: Find Information about how to be trained
- Preventing Suicide: A Technical Package of Policy, Programs, and Practices
- Zero Suicide
- National suicide prevention strategies: Progress, examples and indicators
- Suicide prevention: toolkit for engaging communities
- Understanding Risk and Protective Factors for Suicide: A Primer for Preventing Suicide
- After an Attempt: A Guide for Medical Providers in the Emergency Department Taking Care of Suicide Attempt Survivors
- Responding to Grief, Trauma, and Distress After a Suicide: U.S. National Guidelines
Fact Sheets and Infographics
- 5 Action Steps for Helping Someone in Emotional Pain
- SAMHSA Suicide Prevention Facts & Resources
- Suicide Facts at a Glance
- The National Suicide Prevention Lifeline
- Is Your Patient Suicidal?
- SAFE-T Pocket Card: Suicide Assessment Five-Step Evaluation and Triage for Clinicians
Research Articles
- Tobacco smoking and suicidal thoughts and attempts: Relationships from a general population survey. (Tempier, R. & Guerin, E. 2015. Clinical Epidemiology and Global Health, 3(3), 137 – 143. doi: 10.1016/j.cegh.2014.12.002)
- The Relation Between Nicotine Dependence in Suicide Attempts in the General Population. (Yaworski, D., Robinson, J., Sareen J., & Bolton, J.M. 2011. The Canadian Journal of Psychiatry, 56(3), 161-170. doi: 10.1177/070674371105600306)
- Smoking and Suicide: A Meta-Analysis. (Poorolajal, J. & Darvishi, N. 2016. PLOS ONE, 11(7), e0156348. doi: 10.1371/journal.pone.0156348
- Probing the Smoking-Suicide Association: Do Smoking Policy Interventions Affect Suicide Risk? (Grucza, R.A., Plunk, A.D., Krauss, M.J., Cavazos-Rehg, P.A., Deak, J., Gebhardt, K., Chaloupka, F. J., & Bierut, L.J. 2014. Nicotine & Tobacco Research, 16(11), 1487-1494. doi: 10.1093/ntr/ntu106)
- Heavy tobacco dependence in suicide attempters making recurrent and medically serious attempts. (Lopez-Castroman, J., Cerrato, L., Beziat, S., Jaussent, I., Guillaume, S., & Courtet, P. 2016. Drug and Alcohol Dependence, 160, 177-182. doi: 10.1016/j.drugalcdep.2016.01.004)
- Suicide Prevention Referrals in a Mobile Health Smoking Cessation Intervention. (Christofferson, D.E., Hamlett-Berry, K., & Augustson, E. 2015. American Journal of Public Health, 105(8), e7-e9. doi: 10.2105/AJPH.2015.302690)
- Engagement and abstinence among users of a smoking cessation text message program for veterans. (Christofferson, D.E., Hertzberg, J.S., Beckham, J.S., Dennis, P.A., & Hamlett-Berry, K. 2016. Addictive Behaviors, 62, 47-53. doi: 10.1016/j.addbeh.2016.06.016)
Additional Resources/Information
- National Suicide Prevention Lifeline 1-800-273-TALK (8255)
- Lifeline Chat
- SAMHSA Suicide Prevention Resource Center
- American Foundation for Suicide Prevention
- SAVE (Suicide Awareness Voices of Education)
- American Association of Suicidology
- The Jason Foundation
- Society for the Prevention of Teen Suicide
- National Action Alliance for Suicide Prevention
- National Organization for People of Color Against Suicide
- Now Matters Now
- VA Suicide Prevention
- The Columbia Lighthouse Project
- The Trevor Project
- Tyler Clementi Foundation
This resource digest will continue to be updated as resources are gathered so please keep checking back!
If you have resources/information on this topic that you’d like us to add to this list, please email us at BHtheChange@TheNationalCouncil.org.
Sources
- Tempier, R. & Guerin, E. (2015). Tobacco smoking and suicidal thoughts and attempts: Relationships from a general population survey. Clinical Epidemiology and Global Health, 3(3), 137-143. doi: 10.1016/j.cegh.2014.12.002
- Yaworski, D., Robinson, J., Sareen, J., & Bolton, J. M. (2011). The Relation Between Nicotine Dependence in Suicide Attempts in the General Population. The Canadian Journal of Psychiatry, 56(3), 161-170. doi: 10.1177/070674371105600306
- Grucza, R. A., Plunk, A. D., Krauss, M. J., Cavazos-Rehg, P. A., Deak, J., Gebhardt, K., Chaloupka, F. J., & Bierut, L. J. (2014). Probing the Smoking-Suicide Association: Do Smoking Policy Interventions Affect Suicide Risk? Nicotine & Tobacco Research, 16(11), 1487-1494. doi: 10.1093/ntr/ntu106
- Lopez-Castroman, J., Cerrato, L., Beziat, S., Jaussent, I., Guillaume, S., & Courtet, P. (2016). Heavy tobacco dependence in suicide attempters making recurrent and medically serious attempts. Drug and Alcohol Dependence, 160, 177-182. doi: 10.1016/j.drugalcdep.2016.01.004