It was the 1960’s — walking into your local pharmacy usually meant getting an ice-cold soda pop or a pack of cigarettes, not your prescription. In the same decade, with increased evidence of the ill effects of smoking and rising public awareness, the U.S. Surgeon General released the first report (1964) to examine the health consequences of tobacco use. The report had a significant immediate and long-lasting impact on public attitudes and policies towards smoking, however addictive properties of nicotine were not fully understood at the time and finding effective remedies presented a challenge. Despite research and awareness, the youth of the 1960’s are now older adults in their mid-sixties and older– many of whom are long-term heavy smokers.
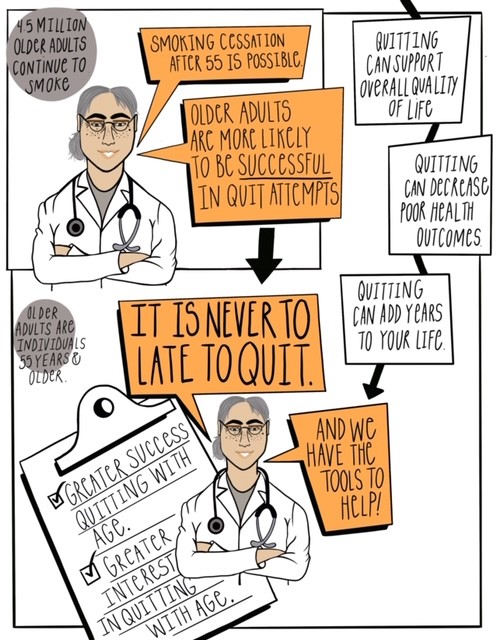 In the United States, nearly 4.5 million adults over the age of 60 continue to smoke, and they account for 70% of all deaths related to smoking. Since the 1960’s (and particularly after the Report of the Surgeon General: 1964 Report on Smoking and Health) there has been significant advancements in tobacco research, control, and cessation efforts; however, tobacco use remains the leading cause of preventable disease, disability, and death.[i]
In the United States, nearly 4.5 million adults over the age of 60 continue to smoke, and they account for 70% of all deaths related to smoking. Since the 1960’s (and particularly after the Report of the Surgeon General: 1964 Report on Smoking and Health) there has been significant advancements in tobacco research, control, and cessation efforts; however, tobacco use remains the leading cause of preventable disease, disability, and death.[i]
Quitting after 60 Still Matters
Older adults who experience greater health challenges with aging and psychological distress, including behavioral health issues, are more likely to be open to quitting.[iv] Research has shown that while older adults are less likely than younger smokers to attempt to quit, they are much more likely to be successful in the cessation attempts they do make, for example:
- While older adults are at greater risk of social isolation, report symptoms of depression, and more likely to smoke, symptoms of depression have been associated with nearly a fourfold increase in smoking cessation efforts among older women.[v]
- Over time, heavy smokers with psychological distress, inclusive of older smokers, smoke progressively fewer cigarettes per day and try to quit in increasingly greater numbers compared to every other group of smokers.[vi]
Cessation Successes and Challenges
It is important for behavioral health providers to remember that smoking cessation beliefs and barriers in older adults can be unique including[viii]:
- Lower confidence in their ability to quit, despite higher success rates when attempted
- Longer history of nicotine addiction
- Perceptions and challenges around medication and pharmacological supports
- Unwanted withdrawal symptoms from chronic use
- Less likely to have received advice and assistance from their physician
- Underestimation of smoking risks, particularly on other chronic conditions
Smoking Cessation Programs for Older Adults
One of the largest challenges around tobacco cessation in older adults is low use of existing cessation programs. Additionally, public smoking restrictions, such as community wide smoking bans, may not have the same impact on the elderly as they do on their younger counterparts due to such policies affecting areas that older adults do not frequent as much (restaurant, bars, work places).[ix]In addition to tailoring cessation efforts towards an aging demographic, targeted cessation efforts should also be inclusive of home, clinical and housing related interventions. For example, cessation support are critical in public housing which serves over two million residents, of which over 329,000 persons are over the age of 62 (16%). Thirty three percent of HUD residents are also current smokers[x], which includes older adults and there is significant room for behavioral health providers to support them. A few additional resources include:
- Self-help interventions for older smokers
- Mobile Smoking Cessation Services
- Smokefree Multi-Unit Housing and Tobacco Cessation
Information for Behavioral Health Providers on Older Adults
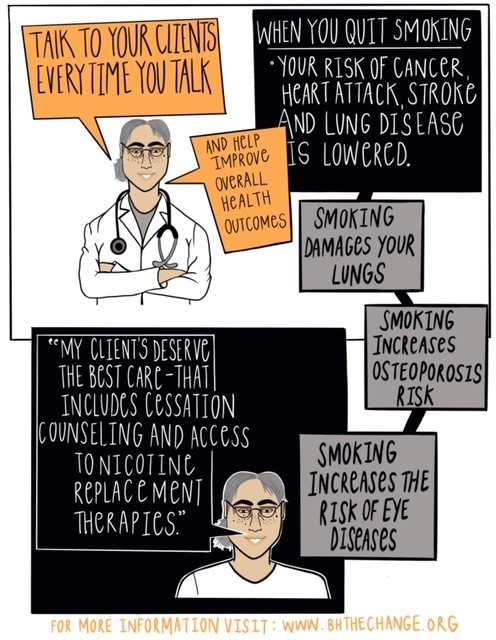
Providing addition information to behavioral health professionals and older adults who smoke on the benefits of smoking cessation at every point in the life course is also important.[viii] Some resources that can be used to understand the needs of, and promote smoking cessation among older adults with behavioral health issues include:
- Fact Sheet from National Institute on Aging: Smoking: It’s Never Too Late to Stop
- Fact Sheet from CAMH: Older Adults & Smoking- Key Messages for Health Care Providers and Policy Makers
- HHS Smoke Free 60+ Infographic: About Smokefree 60+
- HHS Smoke Free 60+ Infographic: Health Effects of Smoking
- HHS Smoke Free 60 + Infographic: What Happens When You Quit Smoking?
- HHS Smoke Fee 60 + Infographic: Household Chemicals in Cigarette Smoke
- HHS Smoke Free 60 + Infographic: Cigarette Substitutes
- NIH Campaign Video: How Does Smoking Affect an Older Adult’s Health?
- Guide from National Cancer Institute: Clear Horizons- A Quit-Smoking Guide for People 50 and Older
To learn more information about supporting tobacco cessation in older adults visit:
- https://60plus.smokefree.gov/
- https://www.bhthechange.org
- https://www.thenationalcouncil.org/about/older-adults/
References