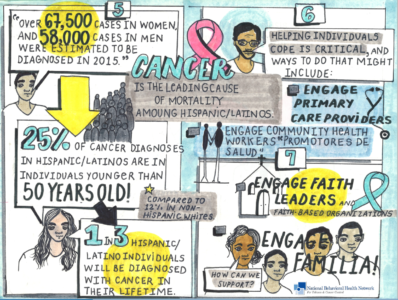
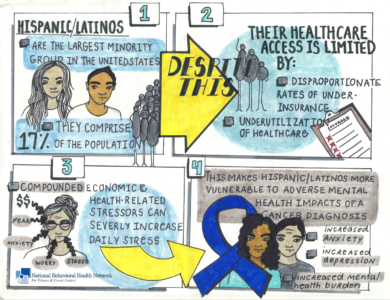
Hispanics/Latinos are the largest minority group in the United States with over 59 million people comprising 18% of the population.[i] However, this growing population’s access to health care is limited by disproportionate rates of underinsurance and underutilization of care[ii], as well as lack of access to providers who speak Spanish and culturally appropriate health services. Even with the implementation of the Affordable Care Act, Hispanics remain the group most likely to be uninsured. In 2016, the uninsured rate for Hispanics was 16% compared with 6.3% among non-Hispanic whites, 10.5% among non-Hispanic blacks, and 7.6% among Asians.[iii] Hispanics are also more likely to struggle with overall economic adversity and have a lower socioeconomic status than non-Hispanic whites which impacts healthcare coverage even further[iv]. Compounded economic and health-related stressors can severely increase daily stress.[v] As a result, research has shown that Hispanics are more vulnerable to the adverse mental health impacts of a cancer diagnosis when compared to non-Hispanic whites. [vi]
 Click Here to download the above inforgraphic created by NBHN.
Click Here to download the above inforgraphic created by NBHN.
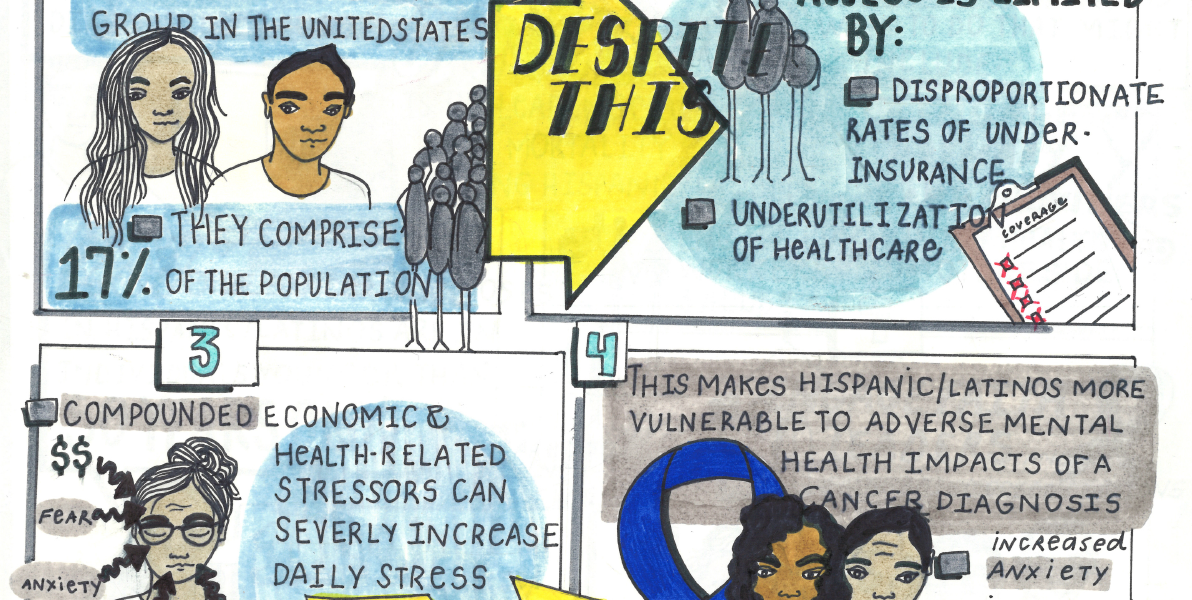
Cancer in Hispanic populations
Cancer is the leading cause of mortality among Hispanics, accounting for 22% of all deaths[i]. Compared to non-Hispanic whites, Hispanics are more likely to be diagnosed with advanced stages of disease and experience poor quality of life following a cancer diagnosis[ii]. Moreover, Hispanics are significantly less likely to be screened for breast, cervical, and colorectal cancers,[iii] and show lower rates of mammography and colorectal testing.[iv] Additionally,
- Over 67,500 new cases in Hispanic women and 58,000 new cancer cases in Hispanic men were estimated to have been diagnosed in 2015[v];
- 25% of cancer diagnoses in Hispanics are in those younger than 50 years of age, compared to only 12% in non-Hispanic whites[vi]; and
- 1 in 3 Hispanic individuals (both women and men alike) will be diagnosed with cancer in their lifetime.
Mental Health Effects of a Cancer Diagnosis
There can be significant psychosocial effects of a cancer diagnosis, especially amongst patients with a pre-existing mental health condition. According to The National Cancer Institute:
- 1 in 3 people with cancer experience mental or emotional distress. [i]
- Hispanics are more vulnerable to adverse mental health impacts due to cancer, when compared to non-Hispanic whites. [ii]
Click here to download the above infographic created by NBHN.
For more research articles on the mental health impacts of a cancer diagnosis in Hispanic populations, see this study from Texas Tech University Health Sciences Center or this study from the Rutgers Cancer Institute.
Managing the psychosocial effects of cancer can be key to ensuring longer survivorship. Evidence-based psychosocial interventions such as cognitive behavioral therapies that focus on stress management, relaxation skills, coping skills, communication skills and social support have been associated with improved emotional well-being, reduced depressive symptoms, and reduced symptom burden among Hispanic patients diagnosed with breast or prostate cancer.[i] These studies have demonstrated consistent areas of improvement in emotional well-being.
Helping Hispanic Patients Cope with the Psychosocial Effects of a Cancer Diagnosis
When seeking to help patients cope with the psychosocial effects of a cancer diagnosis, it is important that providers consider several important factors. First, faith, spirituality, and family involvement are a large part of the Hispanic community’s cultural beliefs. It is important to recognize that these cultural priorities can provide support to patients and play an integral role when interacting with the Hispanic community. Additionally, mental health providers must be aware of and respect that many Hispanics define family differently than other groups. Large, extended Hispanic families should not be misunderstood as over-involved when members show great concern and are involved in a family member’s mental health issues. For example, Hispanics may consider a religious leader to be a member of their family, as well as other non-biologically related individuals, and may wish to have them involved in their care and recovery efforts. [i] Special consideration and accommodation should be given to include all extended family members, as appropriate, in the patient’s care.
Additionally, culturally competent strategies that providers can employ to improve cancer and mental health outcomes in Hispanic patients include:
- Engage community health workers or “promotores de salud”. The use of community health workers (promotores) in community settings has emerged as one of the successful strategies to support the work of health care providers to reduce health disparities in underserved communities. Promotores in Hispanic communities are part of the community they work with and appreciate the values and health experiences of the population they serve. They understand the culture and traditions, speak the language, and have an awareness of the community’s needs.[ii] Promotores are essential in reaching vulnerable, low-income and underserved members of Hispanic populations and work to ensure patients understand their health conditions, make informed choices about treatment and treatment options and encourage adherence to treatment and follow-up.[iii] They also help the patient as their advocate and navigator[iv], and work with community-based organizations to help connect the community to local healthcare and social services.[v] Providers should make integration of promotores in the care coordination team a priority.
- Engage the patient’s primary care provider. Studies have found that a large percentage of Hispanic individuals utilize their primary care physicians and spiritual leaders for their mental health needs[vi]. Efforts should be made to ensure these professionals are identified and included as members of the care coordination team.
- Engage faith leaders/faith-based organizations (FBOs). Faith can play an important role in the health and health outcomes of Hispanic patients. Studies have suggested that Hispanics may rely on clergy and FBOs as the sole source of mental health care. Enhancing collaborations between FBOs and health providers can enhance the effectiveness of FBOs in improving access to treatments for Hispanic patients.
Available Resources for Providers
A variety of organizations focused on addressing both cancer and mental health disparities in the Hispanic community exist and can be used by health providers seeking to better engage the Hispanic community in delivering culturally competent support services. These organizations include:
- Nuestras Voces (Our Voices) National Hispanic Network to Reduce Tobacco-Related and Cancer Health Disparities works toward building Hispanic community infrastructure, as well as increasing partnerships with regional and national tobacco and cancer control networks and other stakeholders, to decrease tobacco use and exposure to secondhand smoke among Hispanics, and increase cancer prevention and management for Hispanics. Through meaningful collaboration and networking, the provision of training and technical assistance, and dissemination of the latest information on tobacco and cancer control, Nuestras Voces empowers Hispanics and those who serve them around the United States to eliminate disparities in these critical health areas. Learn more at www.nuestrasvoces.org.
- National Alliance for Hispanic Health provides science-based health information (in English and Spanish) and advocates for health in the Hispanic community. The Alliance also produces resources on specific cancer topics for Hispanics, such as skin cancer, colorectal cancer, cervical cancer, cancer survivorship, and living healthy lifestyles. Learn more at www.healthyamericas.org/more-resources.
- Redes En Acción is a National Cancer Institute (NCI)-funded initiative to combat cancer among Hispanic populations. The program focuses on developing national and regional networks of partners engaging in cancer research, training, and awareness activities surrounding key Hispanic cancer issues. Learn more at http://redesenaccion.net/publications.
- Latinas Contra Cancer (LCC) was founded to address the void in culturally and linguistically sensitive programs that meet the health care needs of Hispanics around issues of cancer. LCC provides cancer health education, patient navigation and psychosocial family support group services focused on the underserved and low income, Spanish-speaking population. Learn more at http://latinascontracancer.org.
- The National Resource Center for Hispanic Mental Health (NRCHMH) is a 501 (c)(3) dedicated to reducing disparities and increasing treatment quality and availability of mental health services for Hispanics throughout the nation. The NRCHMH also aims to heighten awareness, acceptance and understanding of mental illness among the nation’s Hispanic population. NRCHMH has many resources, including a training video geared to mental health agency administrators and direct service providers who are interested in learning how to better attract and retain Hispanics in professional mental health services. Learn more at http://www.nrchmh.org.
- Dia de la Mujer Latina’s (DML) mission is to motivate, inform, navigate and empower communities at-risk in a culturally and linguistically proficient manner. DML’s signature health and wellness fiesta facilitates early detection screening for breast and cervical cancer and other health challenges (diabetes, etc.) and provides “promotores” (community-based navigators) trained to educate and navigate around health screening and ongoing care and patient case management. Learn more at http://diadelamujerlatina.org
Additional Cancer Resources
For additional information on providing comprehensive mental health care to patients diagnosed with cancer, see NBHN’s earlier blog post: Mental Health Impacts of a Cancer Diagnosis or view our archived Virtual Coffee Chat: Managing the Psychological and Psychosocial Effects of a Cancer Diagnosis.
Need more information? Not a problem.
- View our archived affinity call in collaboration with the Nuestras Voces(Our voices) Network: Best Practices for Supporting Cancer Screening in Hispanic/Latin(x) Clients with Behavioral Health Conditions.
For more information about Nuestras Voces (Our Voices) National Network to Reduce Tobacco-Related and Cancer Health Disparities and its efforts to support Hispanic individuals, families and communities impacted by tobacco use and cancer visit www.nuestrasvoces.org and become a member of the Network.
Additional information to support mental health providers around cancer control in mental health settings, resources including webinars, and opportunities to engage in individualized technical assistance can be found by visiting the National Behavioral Health Network for Tobacco and Cancer Control (NBHN) at https://www.bhthechange.org and becoming a member today!
Blog Authored by NBHN, Nuestras Voces, Tasha Moses and Rachel Landefeld.
Sources
[i] http://www.nrchmh.org/attachments/DoAndDont.pdf
[ii] Rhodes S, Foley Long K, Zometa C and Bloom F. Lay Health Advisor Interventions Among Hispanics/Latinos: A Qualitative System Review. American Journal of Preventive Medicine. (2007). Vol. 33, Number 5, 418-427.
[iii] http://www.apa.org/helpcenter/breast-cancer.aspx
[iv] https://salud-america.org/engaging-latino-families-in-sustainable-mental-physical-and-preventive-healthcare-in-arizona/
[v] Rhodes S, Foley Long K, Zometa C and Bloom F. Lay Health Advisor Interventions Among Hispanics/Latinos: A Qualitative System Review. American Journal of Preventive Medicine. (2007). Vol. 33, Number 5, 418-427.
[vi]Guarnaccia, P.J, Martinez, I, Acosta, H. “Comprehensive In-Depth Literature Review and Analysis of Hispanic Mental Health Issues with Specific Focus on Members of the Following Ethnic Groups: Cubans, Dominicans, Mexicans and Puerto Ricans.” New Jersey Mental Health Institute, Inc. N.d. Web. 20 September 2018. http://www.nrchmh.org/wp-content/uploads/2013/01/FIL5078.pdf
[i] Ashing & Rosales, 2014; Hughes, Leung, & Naus, 2008; Napoles et al., 2015; Penedo et al., 2007
[i] http://ascopubs.org/doi/abs/10.1200/JCO.2014.56.0086
[ii] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4175189/
[i] Cancer Facts & Figures for Hispanics/Latinos 2015-2017 is accompanied by “Cancer Statistics for Hispanics/Latinos, 2015,” a scientific paper published in the American Cancer Society journal, CA: A Cancer Journal for Clinicians.
[ii] Yanez, Betina et al. “Cancer Outcomes in Hispanics/Latinos in the United States: An Integrative Review and Conceptual Model of Determinants of Health.” Journal of Latina/o psychology 4.2 (2016): 114–129. PMC. Web. 19 Sept. 2018.
[iii] Dominguez K, Penman-Aguilar, A, et al. Vital Signs: Leading Causes of Death, Prevalence of Diseases and Risk Factors, and Use of Health Services Among Hispanics in the United States — 2009–2013. Morbidity & Mortality Weekly Report 2015; 64:469–478.
[iv] National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-term Trends in Health. Hyattsville, MD. 2017.
[v] Cancer Facts and Figures, American Cancer Society, 2015. & Figures for Hispanics/Latinos 2015-2017. Atlanta: .
Cancer Facts & Figures for Hispanics/Latinos 2015-2017. Atlanta: American Cancer Society; 2015.
[i] Annual Estimates of the Resident Population by Sex, Race, and Hispanic Origin for the United States, States, and Counties: April 1, 2010 to July 1, 2017 Source: U.S. Census Bureau, Population Division. Release Date: June 2018
[ii] To Address Health Disparities for Latino Youth, Promote Their Engagement in Health Care, Raymond-Flesch, Mariss, Journal of Adolescent Health, Volume 60, Issue 5, 477 – 478
[iii] Barnett, Jessica C. and Edward R. Berchick, Current Population Reports, P60-260, Health Insurance Coverage in the United States: 2016, U.S. Government Printing Office, Washington, DC, 2017.
[iv] Macartney Suzanne, Bishaw Alemayehu, Fontenot Kayla. Poverty Rates for Selected Detailed Race and Hispanic Groups by State and Place: 2007–2011. 2013 Retrieved September 1, 2015, from https://www.census.gov/prod/2013pubs/acsbr11-17.pdf.
[v] Betina Yanez,1 Heather L. McGinty,1 Diana Buitrago,1 Amelie G. Ramirez,2 and Frank J. Penedo, Cancer Outcomes in Hispanics/Latinos in the United States: An Integrative Review and Conceptual Model of Determinants of Health. J Lat Psychol. 2016 May; 4(2): 114–129. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4943845/
[vi] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4175189/